Lipids to Atherosclerosis Essay
Lipids to Atherosclerosis Essay
Recent years the links between lipids and atherosclerosis have been examined.
The main attention is paid to the role of lipids and their influence on the state of health. It was proved that lipids play a significant role in obesity problems and heart diseases. Recent researches have demonstrated that there is a clear relationship between elevated total cholesterol, “bad” cholesterol (or low density cholesterol), blood lipid levels and heart disease. This is specifically important in coronary artery disease, ischemic heart disease, heart attack, congestive heart failure and arrhythmia. Lipids to Atherosclerosis Essay.
ORDER A PLAGIARISM -FREE PAPER NOW
It should be mentioned that lipids are essential as energy stores but also act as structural cell components and vitamins amongst other important functions. They are relatively insoluble in water and are carried in body fluids as soluble protein complexes known as lipoproteins. Plasma lipids are derived from food or synthesised in the body. Genes encoding the key proteins are likely to play fundamental roles in determining plasma levels of cholesterol and fatty acid and thus, susceptibility to atherosclerosis. Therefore, genes involved in lipid are primary candidates as susceptibility genes for coronary atherosclerosis. Atherosclerosis is caused by genetic and non-genetic factors and complex gene-environment interactions.
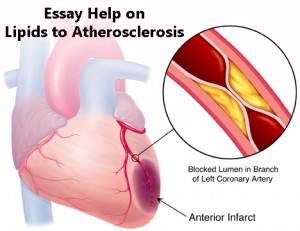
Atherosclerosis is a quintessential complex disease caused by multiple genetic and environmental factors and complex gene-environment interactions and involves multiple vascular territories including coronaries, carotids, and peripheral vessels. It is characterized by vascular obstruction from the deposits of plaque, resulting in reduced blood flow. “Plaque rupture and the consequent thrombosis may lead to sudden blockage of the arteries and cause heart attack. High serum lipid levels, especially the elevated level of low-density lipoprotein have been shown to be strongly related to the development of atherosclerosis”.
Apolipoprotein B is complexed to dietary fats after digestion and is vital for recognition of cell receptors involved in cellular uptake of “bad cholesterol”. It was found that in some diseases, “no apoB is secreted, but atherosclerosis is characterised by high levels of apo B”. More recently it has been shown that disorders of lipid metabolism observed in diabetes and obesity predispose to coronary heart disease.Lipids to Atherosclerosis Essay. Using novel techniques such a DNA microarrays, laboratory models and patient studies, Professor Scott’s team is cloning the genes determining a complex trait of fatty acid transport disorder characterised by raised serum triglyceride levels, insulin resistance, abnormal high density lipoprotein and hypertension. Such a gene may ultimately be a therapeutic target for drugs to treat diabetes. This work also has applications in cancer research, since a novel mechanism of apo B synthesis in the intestine has been implicated in on cogenesis…
Atherosclerosis is the underlying cause of heart attack and stroke. Early observations that cholesterol is a key component of arterial plaques gave rise to the cholesterol hypothesis for the pathogenesis of atherosclerosis. Population studies have demonstrated that elevated levels of LDL cholesterol and apolipoprotein B (apoB) 100, the main structural protein of LDL, are directly associated with risk for atherosclerotic cardiovascular events (ASCVE). Indeed, infiltration and retention of apoB containing lipoproteins in the artery wall is a critical initiating event that sparks an inflammatory response and promotes the development of atherosclerosis. Arterial injury causes endothelial dysfunction promoting modification of apoB containing lipoproteins and infiltration of monocytes into the subendothelial space. Internalization of the apoB containing lipoproteins by macrophages promotes foam cell formation, which is the hallmark of the fatty streak phase of atherosclerosis. Macrophage inflammation results in enhanced oxidative stress and cytokine/chemokine secretion, causing more LDL/remnant oxidation, endothelial cell activation, monocyte recruitment, and foam cell formation. HDL, apoA-I, and endogenous apoE prevent inflammation and oxidative stress and promote cholesterol efflux to reduce lesion formation. Macrophage inflammatory chemoattractants stimulate infiltration and proliferation of smooth muscle cells. Smooth muscle cells produce the extracellular matrix providing a stable fibrous barrier between plaque prothrombotic factors and platelets. Unresolved inflammation results in formation of vulnerable plaques characterized by enhanced macrophage apoptosis and defective efferocytosis of apoptotic cells resulting in necrotic cell death leading to increased smooth muscle cell death, decreased extracellular matrix production, and collagen degradation by macrophage proteases. Rupture of the thinning fibrous cap promotes thrombus formation resulting in clinical ischemic ASCVE. Surprisingly, native LDL is not taken up by macrophages in vitro but has to be modified to promote foam cell formation. Oxidative modification converts LDL into atherogenic particles that initiate inflammatory responses.Lipids to Atherosclerosis Essay. Uptake and accumulation of oxidatively modified LDL (oxLDL) by macrophages initiates a wide range of bioactivities that may drive development of atherosclerotic lesions. Lowering LDL-cholesterol with statins reduces risk for cardiovascular events, providing ultimate proof of the cholesterol hypothesis. All of the apoB containing lipoproteins are atherogenic, and both triglyceride rich remnant lipoproteins and Lp(a) promote atherothrombosis. Non-HDL cholesterol levels capture all of the apoB containing lipoproteins in one number and are useful in assessing risk in the setting of hypertriglyceridemia. Measures of apoB and LDL-P are superior at predicting risk for ASCVE, when levels of LDL-C and LDL-P are discordant. Here, we also describe the current landscape of HDL metabolism. Epidemiological studies have consistently shown that HDL-C levels are inversely related to ASCVE. We highlight recent clinical trials aimed at raising HDL-C that failed to reduce CVE and the shifting clinical targets of HDL-C, HDL particle numbers, and HDL function (e.g. cholesterol efflux capacity). Furthermore, we describe many beneficial properties of HDL that antagonize atherosclerosis and how HDL dysfunction may promote cardiometabolic disease. Lipids to Atherosclerosis Essay.
PATHOPHYSIOLOGY OF ATHEROSCLEROSIS
Atherosclerosis in Cardiovascular Disease
As the underlying cause of heart attack, stroke, and peripheral vascular disease, atherosclerosis is the major cause of death and morbidity in the United States and the industrial world (1). The discovery by Virchow more than 100 years ago that atheroma contained a yellow fatty substance, later identified as cholesterol by Windaus, suggested a role for lipids in the pathogenesis of atherosclerosis (2). Indeed, the goal of this chapter is to focus on the role of lipids and lipoproteins in the pathogenesis of atherosclerosis as well as their critical roles in risk assessment and as targets of therapy. The recognition that atherosclerosis is an inflammatory disease has led to tremendous progress in our understanding of the pathogenesis of atherosclerosis (3). First, we provide brief description of the cellular and molecular events in the key stages of atherosclerosis.
Initiation and Fatty Streak Phase of Atherosclerotic Lesions
The endothelial lining of arteries responds to mechanical and molecular stimuli to regulate tone, (4) hemostasis, (5) and inflammation (6) throughout the circulation. Endothelial cell dysfunction is an initial step in atherosclerotic lesion formation and is more likely to occur at arterial curves and branches that are subjected to low shear stress and disturbed blood flow (atherosclerosis prone areas) (7,8). These mechanical stimuli activate signaling pathways leading to a dysfunctional endothelium lining that is barrier compromised, prothrombotic, and proinflammatory (9). In atherosclerosis susceptible regions, the endothelial cells have cuboidal morphology, a thin glycocalyx layer, and a disordered alignment (8,10,11).Lipids to Atherosclerosis Essay. In addition, these regions have increased endothelial cell senescence and apoptosis as evidenced by ER stress markers (12-14). In contrast, less atherosclerosis prone endothelium is exposed to laminar shear stress causing activation of signaling pathways that maintain endothelial cell coaxial alignment, proliferation, (13,14) glycocalyx layer, (15) and survival (12,16). In atherosclerosis resistant regions, the transcription factors, Kruppel-like factors (KLF) 2 and 4, are activated via MEK5/ERK5/MEF2 signaling which enhances expression of endothelial nitric oxide synthase (eNOS) (17-19). The increased nitric oxide (NO) production promotes endothelial cell migration and survival thereby maintaining an effective barrier (20). In addition, the expression of superoxide dismutase (SOD) is increased to reduce cellular oxidative stress (18). In atherosclerosis susceptible regions, reduced expression of eNOS and SOD leads to compromised endothelial barrier integrity (Figure 1), leading to increased accumulation and retention of subendothelial atherogenic apolipoprotein B (apoB)-containing lipoproteins (low-density lipoproteins (LDL)) and remnants of very low-density lipoproteins (VLDL) and chylomicrons) (21,22). KLF2, KLF4, and NO production inhibit activation of the nuclear factor kappa B (NF‐κB) pathway. Increased NF‐κB activation in atherosclerosis susceptible areas leads to endothelial cell activation (Figure 1), as evidenced by increased expression of monocyte adherence proteins (VCAM-1, ICAM-1, and P-selectin) and proinflammatory receptors (toll-like receptor 2, TLR2) and cytokines (MCP-1 and IL-8) (19,23,24). In addition, endothelial cell activation leads to increased production of reactive oxygen species (25) that can cause oxidative modification of apoB-containing lipoproteins (26). Besides mechanical stimuli, endothelial cell activation is increased by various molecular stimuli, including oxidized LDL, cytokines, advanced glycosylation end products, and pathogen-associated molecules (27-30). In contrast, an atheroprotective function of HDL is to prevent endothelial activation and enhance NO production to maintain barrier integrity (see details below) (31). Lipids to Atherosclerosis Essay.

Figure 1.
Initiation of the atherosclerotic lesion. The fatty streak phase of atherosclerosis begins with dysfunctional endothelial cells and the retention of apoB-containing lipoproteins (LDL, VLDL, and apoE remnants) in the subendothelial space. Retained lipoproteins are modified (oxidation, glycation, enzymatic), which, along with other atherogenic factors, promotes activation of endothelial cells. Activated endothelial cells have increased expression of monocyte interaction/adhesion molecules (selectins, VCAM-1) and chemoattractants (MCP-1) leading to attachment and transmigration of monocytes into the intimal space. Activated endothelial cells also promote the recruitment of other immune cells including dendritic cells, mast cells, regulatory T (T-reg) cells, and T helper 1 (Th-1) cells. The monocytes differentiate into macrophages and express receptors that mediate the internalization of VLDL, apoE remnants, and modified LDL to become foam cells. In addition, inflammatory signaling pathways are activated in macrophage foam cells leading to more cell recruitment and LDL modification.
Immune Cell Recruitment and Foam Cell Formation
Activation of endothelial cells causes a monocyte recruitment cascade involving rolling, adhesion, activation and transendothelial migration (Figure 1). Selectins, especially P-selectin, mediate the initial rolling interaction of monocytes with the endothelium (32). Monocyte adherence is then promoted by endothelial cell immunoglobulin-G proteins including VCAM-1 and ICAM-1 (32). Potent chemoattractant factors such as MCP-1 and IL-8 then induce migration of monocytes into the subendothelial space (33-35). Ly6hi monocytes, versus Ly6lo, preferentially migrate into the subendothelial space to convert to proinflammatory macrophages in mice (36-38).Lipids to Atherosclerosis Essay. The enhanced migration of Ly6hi versus Ly6lo monocytes likely results from increased expression of functional P-selectin glycoprotein ligand-1 (39). In addition, the number of blood monocytes originating from the bone marrow and spleen, especially Ly6hi cells, increases in response to hypercholesterolemia (36). Furthermore, hypercholesterolemia and atherosclerosis increase monocytosis in humans (40,41). Importantly, increased numbers of inflammatory CD14++CD16+ monocytes independently predicted cardiovascular death, myocardial infarction, and stroke in patients undergoing elective coronary angiography (42). Intimal macrophages also result from proliferation of monocyte/macrophages, especially in more advanced lesions (43). During the initial fatty streak phase of atherosclerosis (Figure 1), the monocyte-derived macrophages internalize the retained apoB-containing lipoproteins, which are degraded in lysosomes, where excess free cholesterol is trafficked to the endoplasmic reticulum (ER) to be esterified by acyl CoA:cholesterol acyltransferase (ACAT), and the resulting cholesteryl ester (CE) is packaged into cytoplasmic lipid droplets, which are characteristic of foam cells (42) (Figure 2) (44,45). Modification of apoB lipoproteins via oxidation and glycation enhances their uptake through a number of receptors not down-regulated by cholesterol including CD36, scavenger receptor A, and lectin-like receptor family (see details below) (Figure 2) (46,47). Enzyme-mediated aggregation of apoB lipoproteins enhances uptake via phagocytosis (Figure 2) (48,49). In addition, native remnant lipoproteins can induce foam cell formation via a number of apoE receptors (LRP1 and VLDLR) (Figure 2) (50,51). Uptake of native LDL by fluid phase pinocytosis may also contribute to foam cell formation (Figure 2) (52,53). Lipids to Atherosclerosis Essay.
